Check out our latest #whitepaper containing clinical trial data, real-world evidence, and example algorithms that detail how T2Candida can be incorporated into practice and improve care for invasive candidiasis in your own practice.
Home » Antimicrobial Resistance
AMR occurs when bacteria or fungi obtain the ability to overcome the antimicrobials that have been developed to destroy them. Without any drugs stopping these pathogens, they continue growing, making them difficult or impossible to treat.1
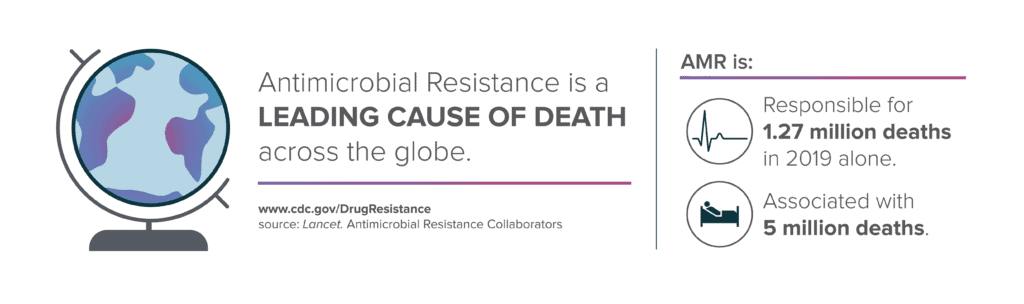
Antimicrobial Resistance is a growing global concern, especially in the wake of the COVID-19 pandemic. According to a study published in The Lancet2, there were 1.27 million global deaths related to antimicrobial resistance in 2019. 73% of those deaths were caused by just six pathogens. Resistant bacteria pathogens can lead to sepsis, and compared to susceptible strains, they are more costly, contribute to longer length of stays, and are associated with higher mortality rates. For example, resistant strains of E.coli, A. baumannii, K. pneumoniae, and S. aureus are at least 2x as deadly3 as their susceptible counterparts, and antimicrobial resistance could cost healthcare systems worldwide $300 billion to more than $1 trillion annually by 2050.4
Any time antibiotics are used, they can contribute to the development of antibiotic resistance. Pathogens survive in plumbing (e.g., sink drains, toilets) and can splash back onto people. Without proper Infection Control, bacteria can spread to people from other people on surfaces like bedrails or the hands of healthcare workers.
Procedures and medical devices (e.g., catheters) can be pathways for bacteria to enter the body, and bacteria can move with patients when they are transferred from one facility to another or even when they are discharged. Resistant infections can also cause infections in the community when they are not stopped in a healthcare setting.5
Current methods for genotypic and phenotypic susceptibility testing rely on positive growth from blood culture, which can take several days. The World Health Organization (WHO) has outlined “better diagnostics” as an essential priority area for fighting back against the spread of AMR, while the CDC states that Antimicrobial Stewardship is one of our best prevention tools against AMR. Culture-independent diagnostics are one way to address the limitations of current diagnostic standards. The T2Bacteria, T2Candida, and T2Resistance Panels provide identification of the most prevalent bacterial and fungal pathogens and genetic markers of resistance within 3 to 5 hours of the first patient blood draw and are independent of blood culture. Results from the panels provide clinicians with critical data needed to influence treatment decisions sooner, often before the second dose of broad-spectrum antimicrobials is administered.
Antimicrobial stewardship is the effort to measure and improve how antibiotics are prescribed by clinicians and used by patients. Improving antibiotic prescribing and use is critical to effectively treat infections, protect patients from harm caused by unnecessary antibiotic use, and combat antibiotic resistance. Stewardship committees are essential to stopping the spread of AMR in healthcare settings.
Initiatives that may be considered by Stewardship Committees:
……………………………………….

Gram-negative marker
KPC
OXA-48 Group
NDM /VIM/IMP
CTX-M 14/15 AmpC(CMY/DHA)
Gram-positive marker
vanA/B
mecA/C
T2 Biosystems, an emerging leader in the field of in vitro diagnostics, is dedicated to saving lives and reducing the cost of healthcare by empowering clinicians to effectively treat patients faster than ever before. T2 Biosystems is focused on addressing critical unmet needs in healthcare starting with sepsis, one of the deadliest and most expensive conditions in hospitals today.
The T2Dx Instrument, the T2Bacteria and T2Candida Panels have received marketing authorization from the U.S. Food and Drug Administration. All other T2 Biosystems products are considered investigational and for research use only.
T2 Biosystems®, T2MR®, T2Bacteria®, T2Candida®, and T2Dx® are registered trademarks of T2 Biosystems, Inc. “T2Biosystems” and the T2 Biosystems, Inc. logo design are registered trademarks or trademarks of T2Biosystems, Inc. All software and documentation is subject to T2 Biosystems, Inc. copyrights. All rights reserved. T2Direct Diagnostics™, T2HemoStat™, T2Plex™, T2Cauris™, T2Resistance™ and T2SARS-CoV-2™ are trademarks of T2 Biosystems, Inc.
© 2022 T2 Biosystems, Inc.
Please tell us where you are visiting from: United States | Outside the United States