Check out our latest #whitepaper containing clinical trial data, real-world evidence, and example algorithms that detail how T2Candida can be incorporated into practice and improve care for invasive candidiasis in your own practice.
Home » Sepsis
Sepsis, the body’s extreme response to an infection, is a global burden on healthcare that affects approximately 1.7 million adults in the United States each year1 and contributes to 11 million deaths worldwide.2 It is also the most expensive hospital-treated condition in the United States, accounting for $62 billion in healthcare costs.3
Bacterial infections cause most cases of sepsis, but fungus, parasites, or viruses can also be responsible. The most common infections leading to sepsis include lung, urinary tract, skin, or gastrointestinal tract infections, which can then manifest in the bloodstream. If sepsis is not identified and treated in a timely manner, it can lead to tissue damage, organ failure, and death.1
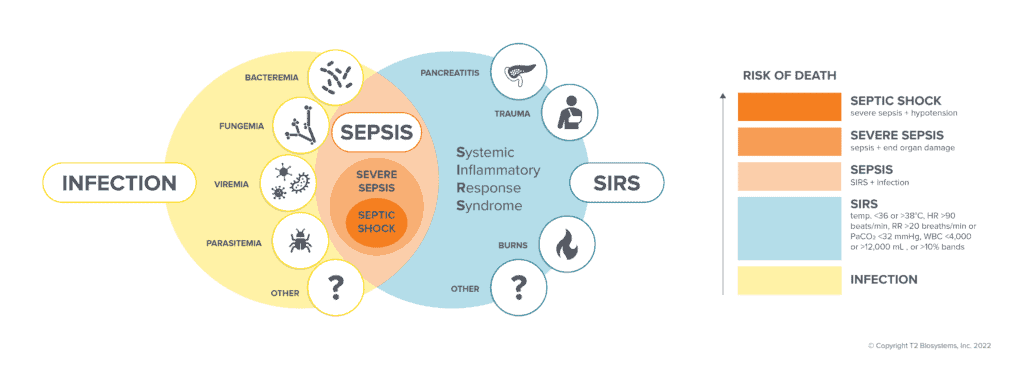
Injury to the body, when severe, can lead to SIRS – the body’s exaggerated defense response to a noxious stressor (infection, acute inflammation, trauma, burns, or other malignancies). The body will try to localize and eliminate the source of insult. A patient is diagnosed with sepsis when the suspected source is an infection, which may lead to more severe conditions and death if left untreated.
Sepsis is suspected when a patient presents with symptoms associated with severe infection, especially if they are in a high-risk category, including infants, the elderly, those with chronic illnesses, and those with weakened immune systems. Common sepsis symptoms include high heart rate, low blood pressure, and altered mental state. fever or chills, shortness of breath, extreme pain or discomfort, or clammy skin.
Severe sepsis occurs when in addition to sepsis, there are also signs of organ dysfunction. Most patients with severe sepsis require treatment in an intensive care unit (ICU). Patients with severe sepsis may further deteriorate into septic shock when their blood pressure drops to dangerous levels. Every hour of delayed treatment for a patient in septic shock increases mortality risk by 8%.5
In addition to symptoms and risk factors, there are several other sepsis screening and assessment protocols (ex. SIRS, qSOFA, MEWS, NEWS, etc.) – a combination of biometrics and physiological measurements that provide clinicians with a score that can be used to assess the risk of sepsis.
Antimicrobial treatment, along with fluid resuscitation, is the most common treatment method for patients with sepsis. For those without a confirmed source of infection, standard guidelines recommend physicians start patients suspected of bloodstream infections on broad-spectrum therapy.6 Broad-spectrum or empiric therapy treats many different organisms but does not necessarily target the specific bacterium or fungus causing the patient’s infection. Blood cultures have long been regarded as the gold standard for diagnosing BSIs, though they can take several days to deliver results.
For patients with sepsis, time is critical – faster time to result and time to targeted treatment leads to improved chances of survival against sepsis.7 While waiting for blood culture results, patient conditions may continue to deteriorate if the broad-spectrum antimicrobial therapy is ineffective against the underlying bloodstream infection. As a result of inappropriate or delayed antimicrobial treatment, patients are at risk of developing potentially life-threatening complications, such as sepsis and septic shock. With millions of people impacted by sepsis every year across the globe, it is critical for physicians to utilize effective diagnostic tools which enable fast initiation of targeted therapy.
Time is of the essence when combatting bloodstream infections and sepsis, making the lengthy nature of the current standard of care problematic. Today’s standard for detecting bloodstream infections includes obtaining blood cultures and waiting for a positive result, which can take between one and five days. Once the culture is positive, subsequent rapid diagnostics may be used for species identification. These post-culture molecular tests take a few hours to produce results after the initial waiting period of one to five days for a positive blood culture.
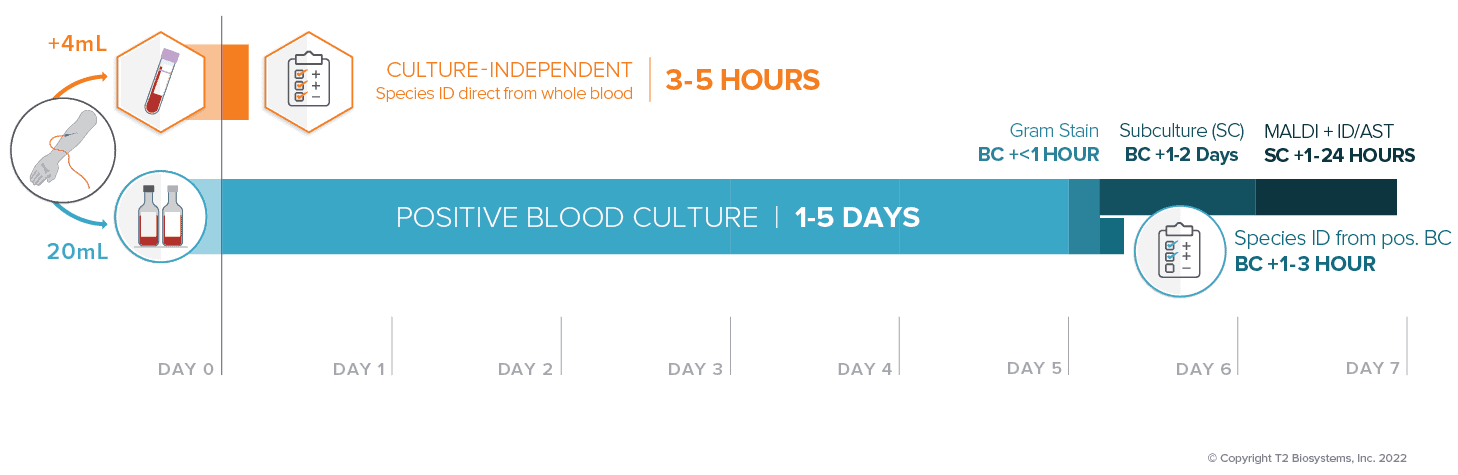
T2 Biosystems has developed the first and only diagnostic test panels to provide species identification directly from a whole blood sample without waiting for a positive blood culture. The T2Bacteria® and T2Candida® Panels are run on the fully automated T2Dx® Instrument and are powered by T2 Magnetic Resonance (T2MR®) Technology.
With results in as little as 3 to 5 hours, physicians can target therapy before the second dose of empiric therapy has been administered. When every hour counts, T2Bacteria and T2Candida can provide rapid species identification for bacterial and fungal infections before the blood culture turns positive, enabling timely and targeted treatment for better patient outcomes.
……………………………………….
T2 Biosystems, an emerging leader in the field of in vitro diagnostics, is dedicated to saving lives and reducing the cost of healthcare by empowering clinicians to effectively treat patients faster than ever before. T2 Biosystems is focused on addressing critical unmet needs in healthcare starting with sepsis, one of the deadliest and most expensive conditions in hospitals today.
The T2Dx Instrument, the T2Bacteria and T2Candida Panels have received marketing authorization from the U.S. Food and Drug Administration. All other T2 Biosystems products are considered investigational and for research use only.
T2 Biosystems®, T2MR®, T2Bacteria®, T2Candida®, and T2Dx® are registered trademarks of T2 Biosystems, Inc. “T2Biosystems” and the T2 Biosystems, Inc. logo design are registered trademarks or trademarks of T2Biosystems, Inc. All software and documentation is subject to T2 Biosystems, Inc. copyrights. All rights reserved. T2Direct Diagnostics™, T2HemoStat™, T2Plex™, T2Cauris™, T2Resistance™ and T2SARS-CoV-2™ are trademarks of T2 Biosystems, Inc.
© 2022 T2 Biosystems, Inc.
Please tell us where you are visiting from: United States | Outside the United States