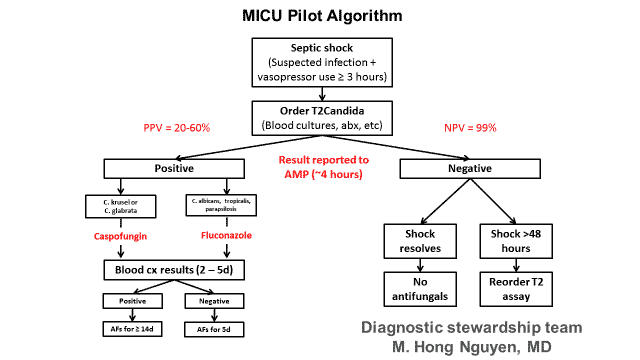
Two 2018 studies from Gregorio Marañón Hospital in Madrid, Spain reported findings of the ability of the T2Candida® Panel to predict patient outcomes:
- Strong indicator of complications: Positive T2Candida Panel results identified patients who had an over 30x increased likelihood of developing health complications, including mortality.
- Strong indicator of poor outcomes: The T2Candida Panel is a better predictor of patients at risk of having poor outcomes than existing diagnostic tests. A negative T2Candida Panel result may significantly shorten the duration of antifungal therapy for 67% of patients.
- Improved distinction between complicated and uncomplicated infection: The T2Candida Panel distinguishes between complicated and uncomplicated infection better than available diagnostic tests.
“The predictive value of the T2Candida Panel represents an important advance in our understanding of the clinical uses of T2Dx diagnostics. A T2Candida Panel positive demonstrated a 30x increase in the likelihood of a complicated infection and showed significant advantages over beta-D-glucan, blood culture and CAGTA,” said Patricia Muñoz, M.D., Ph.D., Division of Clinical Microbiology and Infectious Diseases, Hospital General Universitario Gregorio Marañón, Madrid, Spain. “Together, these studies demonstrate that the T2Dx Instrument is a powerful stewardship tool that can help inform clinicians when they can safely reduce the use of antimicrobial drugs – or when a patient needs more aggressive treatment.”